Introduction
The prognosis for relapsed or refractory Classical Hodgkin Lymphoma (R/R cHL) remains poor, necessitating the development of advanced therapeutic strategies. Brentuximab Vedotin (Bv), a CD30-targeting antibody-drug conjugate, and Bendamustine (B), an alkylating agent, show potential for R/R cHL treatment, yet their individual efficacies have proven only moderate. The putative synergy of the BvB combination on R/R cHL remains largely uncharted, due to restricted sample sizes of existing studies. To address this gap, this meta-analysis is designed to assess response rates and survival outcomes in 527 R/R cHL patients who received the BvB combination as a salvage regimen to enable a curative stem cell transplant.
Methods
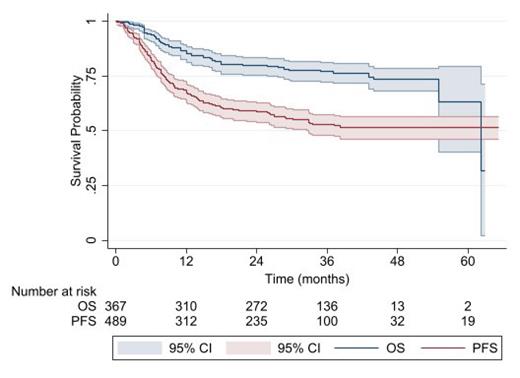
This meta-analysis included patient-level data on adult and pediatric patients with R/R cHL. Individual patient data (IPD) for time-to-event analysis were obtained using the IPDfromKM method. This statistical approach involves reconstructing IPD from the pooled Kaplan-Meier survival curves, allowing for a more comprehensive analysis of patient survival outcomes, including overall survival (OS) and progression-free survival (PFS). Parallel meta-analyses of aggregated data were conducted to determine the overall proportion of patients achieving complete response (CR) and partial response (PR) rates. All statistical analyses were performed using STATA software, version 17. A comprehensive search of clinical trials and real-world data (RWD) was conducted in PubMed and Scopus, including published data until May 2023.
Results
Four clinical trials and 10 observational studies of real-world clinical data were included in this meta-analysis with a total of 527 R/R cHL patients who received the BvB combination therapy. The overall CR and PR rates were 67% (95% CI [63% - 71%]) and 14% (95% CI [11% - 17%]), respectively. The results of CR and PR did not differ significantly between clinical trials and the RWD. BvB response rate was dependent on frontline disease status. The CR rate was higher in relapsed patients (86%, 95% CI [79% - 92%]) than in primary refractory patients (57%, 95% CI [49% - 66%]).
After a median of follow-up of 22 months (12 - 42), the OS was 85.4% (95% CI [81.3% - 88.6%]) at 1 year and 77.1% (95% CI [72.35 - 81.1%]) at 3 years. The PFS at 1- and 3-years was 68.0% (95 % CI [63.5% - 72.4%]) and 53.2% (95% CI [48.1% - 58.0%]), respectively. Among relapsed patients, the 3-year PFS rate was higher at 48.9% (95% CI [33.7% - 62.4%]) compared to primary refractory patients at 29.8% (95% CI [18.6% - 41.8%]); however, the difference did not reach statistical significance (hazard ratio [HR] = 1.59, 95% CI [0.95 - 2.65], p=0.07).
Patients ineligible for ASCT had significantly lower 1-year PFS (41.3% [95% CI: 27.1%-55.4%]) and OS (47.6% [95% CI: 25.7% - 66.7%]) compared to those who underwent ASCT after BvB (PFS: 80.2% [95% CI: 69.2%-87.6%]; OS: 93.8% [95% CI: 84.3% - 97.6%]). Interestingly, the OS was significantly lower in the clinical trials data compared to the RWD (HR= 0.63, 95% CI [0.41 - 0.97], p=0.03).
Conclusions
The BvB regimen demonstrates a notably high clinical response rate and favorable survival outcomes, emphasizing its potential as a valuable rescue therapy, enabling curative stem cell transplantation in patients with R/R cHL.
Disclosures
Otto:yMabs Therapeutics: Consultancy; Cellectar Biosciences: Consultancy.